Conversations about advanced care planning and care through the end of life can be tough when there’s a language gap. And when caregivers can’t mirror a patient’s cultural and ethnic background, that gap can widen.
“What we know from research about caring for underserved populations is that minority patients report better interpersonal care from clinicians of their own race and ethnicity,” said Ira Byock, M.D., founder and chief medical officer of Providence St. Joseph Health’s Institute for Human Caring.
“We also know that non-English speaking patients report better interpersonal care, comprehension, and treatment-adherence with a language-concordant practitioner.”
Ideally, caregivers reflect the communities they serve. When that’s not the case, ACP Decisions videos can help.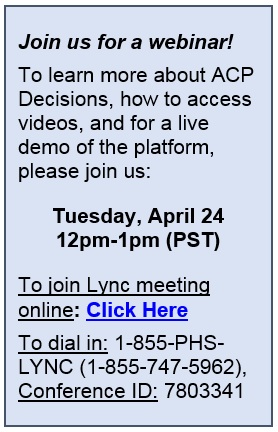
ACP Decisions, a nonprofit physician-founded digital platform, offers evidence-based, videos in many languages. The videos – available for free for all Providence St. Joseph Health caregivers – show what treatments such as cardiopulmonary resuscitation or intubation look like, and walk patients and families through advanced care planning and advance directives.
The videos not only help caregivers reach patients in their own language, they also feature people of their own ethnicity.
Dr. Byock and Dr. Angelo Volandes, co-founder of ACP Decisions, discuss their thoughts on using digital video tools to bridge communication and cultural gaps.
What should Providence St. Joseph Health colleagues know about the videos?
Byock: These high-quality videos are free to all caregivers throughout the Providence St. Joseph Health system. They help bridge communication gaps in non-threatening, easily accessible ways, either at the bedside or at home. They make doing things the right way the easy way – for caregivers, patients and their loved ones.
And we have seen the efficacy of these videos in action. Recently in Western Washington, a health care team used the videos with a family of a 75-year-old Cuban patient. He had heart failure, and been in and out of the hospital. While the nurse spoke Spanish, the videos had a more focused impact on the family, particularly with the decision maker and primary caregiver of the patient, who didn’t understand English and didn’t understand CPR.
After watching the video, the man’s spouse had a better understanding of her husband’s condition, and that there was no definitive cure. Instead, she realized the family and her husband need to address goals of care. The videos aided in this shared decision making.
What insights have you learned about having ACP Decisions videos available in so many languages?
Volandes: How to talk about serious illness and the end of life is different across cultures. Working with native clinicians in non-English cultures has taught us to respect and honor those traditions, cultures and beliefs. Our videos are available in 18 languages and later this year, four more: Urdu, Brazilian Portuguese, Haitian Kreyol, and American Sign Language.
It’s important to honor and respect not only the language surrounding advance care planning in different cultures, but also some of the frameworks in which end of life is understood. Although Americans place emphasis on individual autonomy, considerations of community and family well-being often are critical to any conversation about serious illness in other cultures. Our videos attempt to capture that.
How do ACP Decisions videos help achieve health equality in palliative care and hospice, especially when it comes to the underserved?
Volandes: We know that if you are poor in America, or have low health literacy, or come from an under-represented group, you are unlikely to know about hospice and palliative services. ACP Decisions videos are the equivalent of public health announcements informing patients and families about their options for medical care. Too often in American health care, patients from under-represented groups do not receive hospice and palliative services; the first step to changing that is to empower them with the knowledge of what those services are.
What best-practice advice do you have for caregivers as they use these videos with their patients?
Byock: The videos are not only for patients, but also for caregivers. Most clinicians practicing today finished school more than a decade ago before the age of hospice and palliative medicine. They were never trained in having ‘the conversation’ around serious illness and care through the end of life. They were more likely to have their skills in CPR and performing procedures tested than in having their communication skills sharpened. ACP Decisions videos allow caregivers to be trained in how to have serious illness conversations and improve their skills.
Related to the important work of empowering patients and families to participate in their own health care, describe a moment or story when you knew you were absolutely heading in the right direction with these video tools.
Volandes: I was taking care of a frail, elderly patient with moderate dementia. She was in her late 80s and I was admitting her to the hospital. When her daughter eventually came to the hospital, I sat down with her to talk about her mother’s goals of care. She looked at me and began to cry because she was so overwhelmed. “Nobody taught me any of this; I am just supposed to know how to make all these decisions? I am not a doctor…”
I had a long conversation with her and realized that we place such a decision making burden on the children of our patients, yet we as doctors do nothing to train them on how to make decisions. We sat down and saw a series of videos from our suite of videos for the family members of patients with dementia. We talked about best interests and what her mother would have wanted. We also discussed her goals of care and saw the two videos that covered decision making and goals of care. Although the daughter’s decision were not by any means easy to make, she felt better prepared.
Questions?
For questions regarding ACP Decisions, contact the Institute for Human Caring, HumanCaring@providence.org.
Other stories of interest:
Get your new (and free!) Providence St. Joseph Health advance directive toolkits